 |
| Chevron boarder: http://coffeekidsandcompulsivelists.blogspot.com.au/ |
As April is Autism Awareness Month, I thought over the next four weeks, I would take time to write about one of things I LOVE about being an SLP, working with children with Autism Spectrum Disorders (ASD)! I know many of you SLPs reading this out there are familiar with many of these topics. However, as I have regular educators, parents and even grandparents who follow me, I will be discussing topics that not all readers may be familiar with.
In this post, I am writing under the assumption that those who are reading this understand what ASD is and what it looks like. If you are not familiar with autism spectrum disorders, I encourage you to stop reading this right now and head on over to Autism Speaks and Autism Action Partnership for more information. Then come on back and read about DTT!
Firstly, let me say that I do not believe that there is a "one size fits all" approach to treating children with ASD. I believe there are a number of valid techniques that can work for children with ASD. There are several factors that may affect your decision on which techniques to try: 1) severity of disorder and use of stimulatory behaviors, 2) sensory needs of the child, 3) family needs, 4) parental support, etc.. I tend to use evidence based practice (EBP) and trial and error to determine "what works" for each child on an individual basis.
Over the next five weeks we will be discussing topics such as discrete trial training (today), use of DTT principles with a penny board, DIR/Floortime/PLAY project principals, ABA vs. Son-Rise program and sensory diets. So...let's get started!!!!
What is DTT?
DTT or discrete trial training is a method of teaching small components/steps of a skills. It is a method often used successfully when providing intervention to persons with ASD. DTT is only one technique used in ABA (applied behavioral analysis) therapy. DTT has an extensive body of research (website courtesy of Autism Speaks Blog) to support its use and success.
Word of Caution: I would be remiss if I did not point out that upon review of research on past ABA studies, there have always been criticisms about the methodologies used in these studies and more recently, there are valid questions as to whether these research studies truly demonstrated the results they claimed. In addition, the difficulty and/or lack of generalization of learned skills to more natural environments has always been a concern for those who question the use of ABA. With that said there are thousands upon thousands of success stories (anecdotal research) of children who received ABA therapy and thousands of stories of children where ABA did not work. So I just make these statements to let you know, there are children who can and have improved using these techniques and ones who haven't. No one seems to know why some children respond to ABA techniques when others do no. You as a professional or parent must conduct your own research and make your own decisions regarding the child's direction of therapy.
Want to read more about the critiques of ABA? Check out: A Case Study in the Misrepresentation of Applied Behavior Analysis in Autism: The Gernsbacher Lectures for more information and as always...you decide!
Ok now let's get down to talking about DTT!
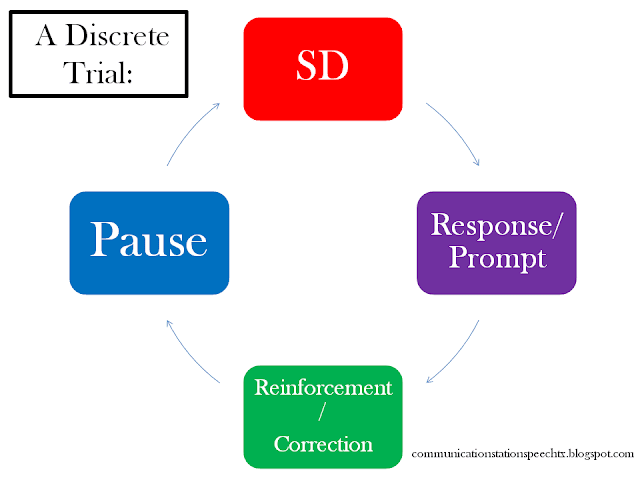
What is a discrete trial? One discrete trial consists of:
- An SD: discriminative stimulus, otherwise known as the instruction (verbal, nonverbal-pointing/showing, physical-hand over hand, guide hand, etc.) given by the therapist to the child. All SDs should be:
- consistent and clear
- free of extraneous information (includes visual, auditory, kinesthetic info, etc.)
- slightly louder than normal speaking tone
- Response or Prompt: Then the therapist waits for the child to respond, or provides help by prompting a response; follow hierarchy from MOST amount of scaffolding to least amount of scaffolding and must fade prompts (either by decreasing intensity of prompt or by checking to see if child is ready to move to next level of prompting); prompts include:
- physical-hand over hand, guide hand, etc.,
- modeling,
- gestural-pointing, showing,
- positional-positing materials to encourage correct response,
- verbal-vocal cues to help child,
- echo prompts-you prompt verbal answer immediately after stimulus and have child echo
- Reinforcement or correction: Finally, (after the child's response), the child is given reinforcement for a correct response, or correction for an incorrect response.
- reinforcement:
- MUST be given immediately
- IS GIVEN regardless of whether the child responded independently or with a prompt
- should be exciting and motivating
- should be varied (decreases boardem an sustains motivation)
- What to do if the child responds incorrectly or not at all? 2 options:
- Informational "No": say no in a neutral tone, exhibit stimulus again, provide model for correct response, when child imitates correct response, reinforcement follows. OR
- Errorless learning correction: the therapist does not say "no" but rather pauses (does not provide reinforcement), give stimulus again, immediately modeling correct response, after child gives correct response, reinforcement is given.
Want a copy of the above graphic for your reference? You can download it here!
What is a reinforcer and how do I determine what to use as reinforcement?
A reinforcer is anything that is motivating to the child and signals to him/her that the response made was correct. I like to take a preference inventory when I first meet new clients. I ask the child's parents what types of toys, cartoon characters, snacks, physical touch, activities, praise, and sensory toys the child seems to enjoy. This will provide me with a guide to determine possible reinforcers for each individual child.
Tokens or counters can also be used for reinforcement. Usually this technique is used only for children who are familiar with DTT for the purposes of delaying and fading out reinforcement (as child has to obtain several tokens/counters in order to obtain the reinforcer).
Note: If the child has a sensory aversion to various textures, sounds, or visual stimuli, DO NOT use objects that exhibit those aversions as this will not be reinforcing for the child.
Positives to using DTT and/or ABA therapy: (overview-there are many more than listed here)
- research shows consistent progress for various children
- new skills can be taught in steps
- undesireable behaviors are extinguished using negative consequences
Negatives to using DTT and/or ABA therapy: (overview-there are many more than listed here)
- difficulty generalizing to other environments
- reliance on cues and prompts
- use of robotic speech
- skills taught may not be functionally observed in the child's daily environment
- negative consequences are viewed as harsh in nature
With such high caseloads, is this really something an SLP can do in the school setting?
First off let me state that educators in the school environment are bound by FAPE (free and appropriate education) and are expected to provide services in the LRE (least restrictive environment) for EVERY student. LRE means that the student should remain in the classroom setting as much as possible and only be removed when that skill/service etc. cannot effectively be taught/provided within that setting. LRE can also be interpreted to mean that the amount of service a student receives outside of the classroom should be NO MORE than the amount the student requires to make progress (the amount of progress or speed of progress will vary on an individual basis depending on numerous factors: age, developmental level, cognition, co-morbid disorders, family support, etc.). This is does not mean a student should spend the entire school day in a therapy room one-on-one with any therapist or special educator participating in hours of discrete trials. If this is what you want as a parent, than you should think about seeking ABA therapy outside of the school day (keeping in mind that schools are not responsible for services outside of the school day). In addition the goals targeted within the school environment MUST RELATE to the skills the child will need to successfully navigate within that academic environment. That is the law. Private practice/out-patient services can relate to services in the school environment but are bound by different regulations and laws which is why services in and outside of the academic environment look so different.
So DTT cannot be done in the school setting?
With that said, as a school SLP it is quite tricky to say the least, to carve out time for one-on-one individualized sessions let alone hours of therapy. However, for the appropriate students (the students low functioning where use of DTT principals was necessary to make progress), I could ONLY do this with the support and collaboration of the multidisciplinary members. I worked closely with the child's special education teacher, classroom paraprofessionals, and occupational therapist. And between all of us we were able to provide meaningful daily work periods of with some activities based on DTT principles for students (periods may only have been 15-30 mins depending on the students attention skills, cognition abilities, severity, etc.). Of course this was not equivalent to the number of hours a child with ASD would receive via ABA therapy a week (although there is still some debate on the number of recommended hours of ABA therapy), nor should it be, based on federal law and LRE. In addition, what tasks were taught were directly related to academic skills, behaviors, and curriculum. Therefore with relatively fewer DTT principal based sessions/activities we as the multidisciplinary team, were able to teach skills AND encourage carryover into the classroom setting with fair consistency.
So I suppose my short answer is, DTT principals can be used to effectively teach children with ASD in various settings. However the length of time and ability with which to provide DTT principal-based activities will change based on the setting we are providing these services (school, private practice, outpatient hospital, home, etc.).
The last thing we must remember is that ONLY TRAINED professionals should be providing ABA within their sessions. As you can see above I do not claim to have provided ABA but rather, I have used DTT principles on which I have based my activities to support children as needed. It is unethical to expect a professional untrained in this area to provide these services to your child.
Join me next week when I talk about how I use some of these principals in a modified activity with a penny board in order to teach academic skills/behaviors and how, as working with a team, we were able to generalize these skills to the classroom environment making a child with ASD more functional in nature.
References:
- Autism Intervention Training Videos (you can find these on youtube.com)
- Educate Autism: Discrete Trial Training
- Autism Speaks Blog: Discrete Trial Training


GREAT post!!
ReplyDeleteThank you! I appreciate your comment. I have to admit some of these topics this month were somewhat difficult to write as they are so involved and it is difficult to determine how much information to add before it becomes too confusing or overwhelming. So it helps to hear a positive comment for sure! Thanks so much :)
Delete